Home > All Blogs > Connection Between HPV and Cervical Cancer
Connection Between HPV and Cervical Cancer
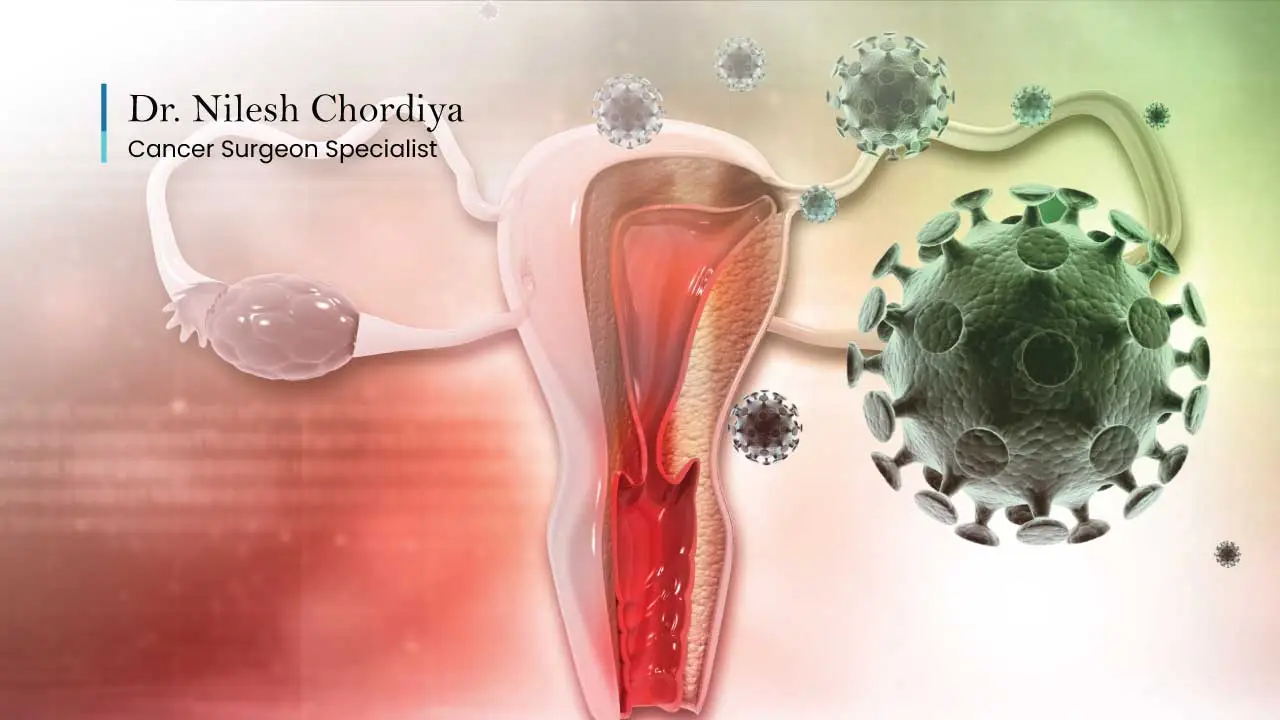
Cervical cancer is almost always caused by an infection with a virus called human papillomavirus (HPV).
This virus spreads through close, skin-to-skin contact, often during intimate moments, and over time it can turn healthy cervical cells into cancer.
The good news is that cervical cancer is preventable if caught early, thanks to vaccines and regular screenings.
This article will explore:
- What is HPV and how is it linked to cervical cancer?
- Who is at risk and how does HPV spread?
- How can you prevent cervical cancer caused by HPV?
- What are common myths and facts about HPV?
- How screenings and vaccines play a major role in prevention.
I’ll walk you through this step by step, offering clarity and addressing concerns commonly brought up by patients.
What Is HPV?
HPV, or human papillomavirus, is a group of more than 100 related viruses. Some types can cause harmless skin warts like those on your hands or feet, but it’s HPV’s high-risk types that concern us when it comes to cervical cancer. These types can infect cells in the cervix and, over time, cause changes that may lead to cancer.
How Does HPV Cause Cervical Cancer?
To put it simply, HPV causes damage on a cellular level.
Imagine a scratch on your skin that heals quickly. Now, picture if the scratch doesn’t heal properly and the skin starts changing strangely due to an infection.
That’s what HPV does within the cervix. If left unchecked for years, these changes can develop into cervical cancer.
Almost all cervical cancers (over 95%) are directly linked to high-risk HPV types, particularly types 16 and 18. These two are the culprits in nearly 70% of all cases.
Is HPV Common?
Yes, it is incredibly common. Nearly everyone contracts it at some point in their life, often without even knowing. Most of the time, your immune system clears the virus within a year or two. For those with long-lasting infections involving high-risk types, the risk of cervical cancer increases.
One of my patients, a 35-year-old woman, came to me after her routine Pap smear showed abnormal cells. She wasn’t experiencing any symptoms. Tests confirmed a high-risk HPV infection.
Because she was vigilant about her screenings, we caught the changes early and treated them before they progressed further. This highlights the importance of regular check-ups.
Need help? Talk to Our Cancer Surgeon
Get the Most Effective Cancer Treatment in India by Consulting Dr. Nilesh Chordiya, One of the best Cancer surgeons in mumbai.
Who Is at Risk of HPV and How Does It Spread?
How Does HPV Spread?
HPV spreads through direct skin-to-skin contact, often during vaginal, anal, or oral sex. Interestingly, it doesn’t always require penetration for the virus to transmit. This is why using protection like condoms lowers, but doesn’t completely eliminate, the risk.
Who Is Most at Risk?
Anyone who is sexually active can be exposed to HPV, but some individuals are more vulnerable to persistent infections and complications:
- Younger people, as their bodies are often just starting to encounter the virus.
- Women with weakened immune systems, like those with HIV or on immune-suppressing medications.
- Women who haven’t had regular cervical screening tests.
- Long-term smokers. Tobacco chemicals can damage cervical cells, making it harder for the body to clear the virus.
It’s worth mentioning that partners can unknowingly pass the virus since it doesn’t always show symptoms right away.
Men and HPV
Men are not exempt. High-risk HPV types can cause cancers of the throat, anus, and penis in men, although these are less common compared to cervical cancer in women. Encouraging HPV vaccination for boys and men can break the chain of infection.
How Can Cervical Cancer Be Prevented?
Preventing cervical cancer involves being proactive through vaccination and routine screenings.
1. Get Vaccinated Against HPV
The HPV vaccine has been a game-changer in reducing cervical cancer cases. It is most effective when given before someone becomes sexually active and exposed to the virus.
⇒Who Should Get the Vaccine?
- For children and teenagers aged 9-14, this is the recommended age group for vaccination.
- Young women up to age 26 and men up to age 21 can also benefit if they missed vaccination earlier.
- Adults aged 27-45 can discuss vaccination options with their cancer doctor to see if it’s suitable.
2. Regular Screenings
Screening for cervical cancer ensures abnormal cells are caught long before they become cancerous. There are two primary tests:
- Pap smear (Pap test): Looks for changes in cervical cells caused by HPV.
- HPV test: Specifically checks for high-risk types of HPV.
For women in Mumbai or Thane, booking routine tests with your gynecologist can make all the difference. Early detection saves lives.
⇒How Often Should You Be Screened?
- Women from age 25 to 65 should have regular screenings.
- If both an HPV test and Pap smear are negative, screenings can continue every 5 years.
3. Healthy Lifestyle Choices
- Quit smoking: Smoking makes it harder for your body to fight off HPV infections.
- Practice safer sex: Use condoms and limit the number of sexual partners to reduce exposure risk.
- Strengthen your immune system: A balanced diet, exercise, and adequate sleep all help your body fend off infections like HPV.
Myths and Facts about HPV
Myth 1: HPV Always Leads to Cancer
Fact: Most infections clear on their own and don’t cause cancer. Regular follow-ups ensure early treatment if needed.
Myth 2: Only Women Need the Vaccine
Fact: Men benefit from the vaccine by reducing their risk of HPV-related cancers and lowering their chances of transmitting the virus.
Myth 3: HPV Only Spreads If You’re Promiscuous
Fact: HPV can infect anyone who is sexually active. Even someone with one lifelong partner could contract the virus if their partner was exposed.
Myth 4: You Don’t Need Screening if You’re Vaccinated
Fact: While vaccination greatly lowers your risk, it doesn’t cover all cancer-causing HPV types. Screening remains essential.
When Should You See a Doctor?
Some patients only come in when symptoms emerge, such as unusual bleeding, pelvic pain, or abnormal discharge. These can indicate advanced cervical disease. However, relying on symptoms isn’t wise since cervical pre-cancer often has no symptoms at all.
If you:
- Haven’t been screened in the past 3 years.
- Are unsure about vaccination or want more advice.
- Have concerns about symptoms, contact your gynecologist or a specialist like myself.
Taking Action Today
Cervical cancer is preventable if you take the right steps. Start by:
- Ensuring regular Pap and HPV tests as recommended.
- Encouraging vaccination for yourself or your children.
- Adopting lifestyle changes to improve overall health.
If you’re in Mumbai or Thane, I am here to assist with your concerns. From screenings to treatment options, every step is taken with empathy, understanding, and your health in mind. Take charge today; early protection is your best defense.
APPOINTMENT FORM

About Author
Related Blogs
Cervical Cancer vs. Uterine Cancer: What Is the Difference?
Cervical cancer starts in the cervix from HPV, while uterine cancer begins in the uterus lining due to hormonal imbalance.
How Long Can You Have Cancer Without Knowing?
You can have cancer for months or years without symptoms. Learn why early detection and routine check-ups are key to staying safe and healthy.
Cervical Cancer Vaccine Cost in India
Cervical cancer vaccine in India costs ₹2,000–₹10,000 per dose. Free or low-cost options available via govt programs and Cervavac.


